코로나19 감염병 전담병원 간호사의 근무실태, 지원체계의 적절성 및 간호 전문직 자부심
Working Status, Adequacy of Support, and Nursing Professional Pride among Frontline Nurses at a Designated COVID-19 Hospital
Article information
Abstract
목적
본 연구는 코로나 감염병 대유행 상황에서 코로나전담병원에 근무하는 간호사들의 근무현황, 국가 및 지방자치단체의 지원체계 적정성 및 간호전문직 자부심을 조사하기 위하여 시도되었다.
방법
대구에 소재한 코로나전담병원에 근무하는 첫 대유행 기간 동안 근무한 간호사 157명을 대상으로 2021년 1월 15일부터 2월 15일까지 조사한 서술적 횡단연구이다. 설문지를 통해 근무현황, 국가 및 지방자치단체의 지원체계 적정성 및 간호전문직 자부심에 대하여조사하였으며, 자료는 기술통계로 분석하였다.
결과
간호사는 인력부족으로 월 7-8일, 하루 2.06시간 초과근무를 하였으며, 간호사의 97.5%가 전염에 대하여 두려움을 나타내었다. 또한 간호직무의 감염위험성에도 불구하고 국가 및 지방자치단체의 지원이 부족하다고 응답하였다. 간호전문직 자부심은 평균 3.44점으로 90% 이상의 간호사가 간호사의 전문성 향상을 인지하였다.
결론
과중된 업무에도 일선의 간호사들이 제대로 보상받고 있지 못함을 시사하며, 이를 개선하기 위한 정책이 수립되어야 한다.
Trans Abstract
Objectives
The purpose of this study was to investigate experiences such as working status, adequacy of support system from the nation and local government, and nursing professional pride of nurses working at a Coronavirus disease-2019 (COVID-19) designated hospital during the early COVID-19 pandemic in Daegu Metropolitan City, South Korea.
Methods
This study was a cross-sectional study. Participants were 157 nurses who cared for 851 patients with coronavirus infectious disease during the initial pandemic from February 18 to May 18, 2020. Work-related characteristics, national/local government/institutional support provided for risky nursing care, and nursing professional pride (Korean-Nursing Professional Pride) were surveyed from January 15 to February 15, 2020. Data were analyzed by descriptive statistics.
Results
Nurses worked 21 to 22 days with 7 to 8 days of overtime working a month and 2.06 hours of overtime working a day due to a shortage of nursing staff. Of them, 97.5% of nurses demonstrated concern about the transmission of COVID-19. Despite the working conditions, many participants perceived national and local government support systems for challenging works as insufficient. However, the nursing professional pride was 3.44, and more than 90% of nurses perceived increased professional awareness of nurses.
Conclusion
This study suggested that frontline nurses were overworked due to the explosive increase of patients and inadequately compensated, and policies should be established to improve these issues.
INTRODUCTION
The novel coronavirus disease-2019 (COVID-19), declared a pandemic by World Health Organization (WHO), is an ongoing respiratory infectious disease [1]. South Korea was initially affected by COVID-19 due to its geographical proximity to China [2]. When the first pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported on December 31st, 2019, in Wuhan [3], the Korea Disease Control and Prevention Agency (KDCA) issued the lowest threat alert (blue) of 4 levels. Despite the confirmed cases that occurred sporadically, they seemed to be controlled stably by tracking case movement routes, rapid diagnosis, and widespread testing [4]. However, things changed abruptly when the 31st case occurred in Daegu Metropolitan City with 2.5 million people located inland of South Korea, on February 18th, 2020 [5]. As the mass infection was confirmed to be centered on the specific church where the 31st case participated, the Korean government immediately started an active response by raising the alert system to the highest threat alert (red) [4,6].
Daegu Metropolitan City has reorganized the ten local hospitals as designated COVID-19 hospitals for the increasing number of infected patients management [5]. However, as the number of patients waiting for other hospitals increased because the isolation ward could not accommodate all infected patients with the rapidly increasing number of confirmed COVID-19, designated COVID-19 hospitals transferred existing inpatients to another hospitals sequentially in order to treat COVID-19 entirely [7]. Among the hospitals, a regional district public hospital (Daegu Medical Center), most of the nurses were assigned to isolation ward for an infected patient that was completely different from their existing duties except for artificial kidney rooms, hospice centers, and minimal outpatients with volunteer medical staff from all over the country [7,8]. These changes in the medical system directly and/or indirectly affected frontline nurses [9]. In particular, nurses’ work was aggravated due to mass cluster outbreaks in the psychiatric and long-term care and poor treatment of dispatched nurses [10]. In addition, nurses who were fighting COVID-19 have experienced dehydration and exhaustion due to wearing Personal Protective Equipment (PPE), a dilemma in an ethical conflict situation, and threatening their mental health such as anxiety, depression, burnout, and post-traumatic stress disorder [10–12].
Currently, nurses worldwide are writing a new history of nursing against a novel infectious disease. Like Nightingale, medical staff, including nurses, are portrayed as heroes or martyrs and are praised by the public for their hard work [13]. However, existing studies on the experiences of nurses while caring for patients with a COVID-19 show the need to improve the treatment of nurses in the future, such as the caring difficulties for novel diseases [14,15], extended working hours [16], and stress [17]. Although nurses are dedicated to caring for infected patients and the working experience of nurses, it is necessary to look at the driving force and pride that keep them working. Therefore, this study was conducted to examine the experience and professional pride of the frontline nurses who treated the explosively increasing number of patients during the first wave in the absence of a proper medical system for emerging infectious diseases. Through this, it is intended to be used as primary data for preparing nursing support policies in an infectious disease outbreak.
METHODS
Study design
This study is a descriptive, cross-sectional survey to explore the experiences and professional nursing profession pride of nurses who worked at a designated hospital dedicated to COVID-19 during the early pandemic from Feb 18 with the first confirmed case to May 18, 2020, when the number of infected patients increased explosively.
Setting and sample
The study participants were 157 nurses who work at the designated COVID-19 hospital, understand the purpose of the study, and agreed to participate in the study. The study subjects were selected as nurses who had more than six months of work experience during the first pandemic of about three months from February 18, when Daegu Metropolitan City's first confirmed coronavirus case was hospitalized, to May 18, when 6,871 patients were recorded.
During the first pandemic, approximately 290 nurses were employed in the designated COVID-19 hospital, and questionnaires were distributed after explaining the purpose of the study and obtaining consent to participate in the study from 170 people that excepting 29 dispatched nurses, 15 of whom did not take direct care of COVID-19, and 26 who later resigned. A total of 160 questionnaires were retrieved, showing a response rate of about 98%, and 157 of them were used for final analysis, except for three questionnaires with unanswered items.
Instruments
Working status and adequacy of support
In order to understand the experiences of nurses who work at the designated COVID-19 hospitals, three nurses with more than nine years of clinical experience and two nursing professors developed the questionnaire. The final questionnaire was determined after revising through a pilot survey. First, the general characteristics of nurses consisted of age, gender, education, a department where they worked before, position, duration of working, educational background about infection control, nursing experience for infected patients, and training experience in wearing PPE. Second, regarding experiences of working status, it consisted of 13 items, including the number of working days, day-off per a month, day of overtime work per a month, hours of overtime work per a day, shift work, transfers to another department, and most time-consuming nursing work, most challenging nursing work, most memorable things, adequacy of work-sharing, driving force to continue to work, and concerns about infection of COVID-19. Third, to investigate the experience of the support system of the nation, local government, and affiliated institution, seven items were measured re-education about infection control and wearing PPE, the usefulness of national/local governmental/institutional guidelines, the sufficiency of national/local governmental/institutional support, adequacy and timeliness of the compensation for overtime work, and adequacy and timeliness of compensation for risky nursing work.
General characteristics of COVID-19 patients
In order to understand the nurse's working situation, seven questions were investigated about the age, gender, comorbidities, symptoms of admission, length of hospital stay, facilities of confirmation, and clinical outcomes of COVID-19 patients admitted during the first pandemic.
Nursing professional pride
Nursing professional pride was measured by the Korean version of the Nursing Professional Pride (KNPP) scale, and one question asking about subjective awareness of nurses through the COVID-19 pandemic is improved. The KNPP scale was developed by Jean et al. [18] and consists of a total of 27 items that measure the feeling of vocation (6 items), the role satisfaction (6 items), role of problem-solver (6 items), self-achievement (4 items), and willing to stay (5 items). Each item was answered with a Likert 5-point scale ranging from ‘ strongly disagree’ (1 point) to ‘ strongly agree’ (5 points), and the higher the measured score, the higher the pride of nursing professionals. The internal reliability was Cronbach's α was 0.92 at the development and was 0.94 in this study. The reliability of the sub-factor with Cronbach's α was vocation was 0.85 and 0.81, role satisfaction was 0.81 and 0.89, the role of problem-solver was 0.93 and 0.83, self-achievement was 0.82 and 0.83, and willing to stay was 0.74 and 0.77 at the time of development and in this study, respectively.
The subjective feeling of whether or not the professional perception is improved was asked, ‘ Compared to the situation before the coronavirus pandemic, do you think the general public's professional perception of nurses has improved?’ and responded with a 4-point Likert scale from ‘ strongly disagree’ (1 point) to ‘ strongly agree’ (4 points).
Data collection
Data were collected from January 15 to February 15, and the medical record survey of COVID-19 patients was from March 15 to 31, 2021. In order to understand the working status of nurses who directly participated in the nursing of COVID-19 patients, the disease characteristics of 851 COVID-19 patients admitted to the designated COVID-19 hospital during the first pandemic of 3 months were investigated. After obtaining approval to view medical records at the hospital, three research nurses and five nurses prepared a survey based on medical records.
Data analysis
For the collected data, 157 copies of the questionnaire for nurses and data of 851 COVID-19 patients were finally analyzed using the SPSS 25.0 (IBM Co., Armonk, NY, USA) program. The subject's general characteristics, general characteristics and disease characteristics of COV-ID-19 patients, work status and support system and nursing professional pride were analyzed by descriptive statistics of frequency, percentage, mean and standard deviation, minimum and maximum.
Ethical considerations
Before data collection, it was approved by the Institutional Review Board of the Daegu University (No. 1040621-202009-HR-023), and data on nurses and COVID-19 patients were collected after approval of the hospital's research and medical records. Research explanations were provided to the study subjects to guide them on the purpose of the study, confidentiality, and data storage deadline, and to ensure autonomy in participating in the study.
RESULTS
General characteristics of nurses working at a COVID-19 designated hospital
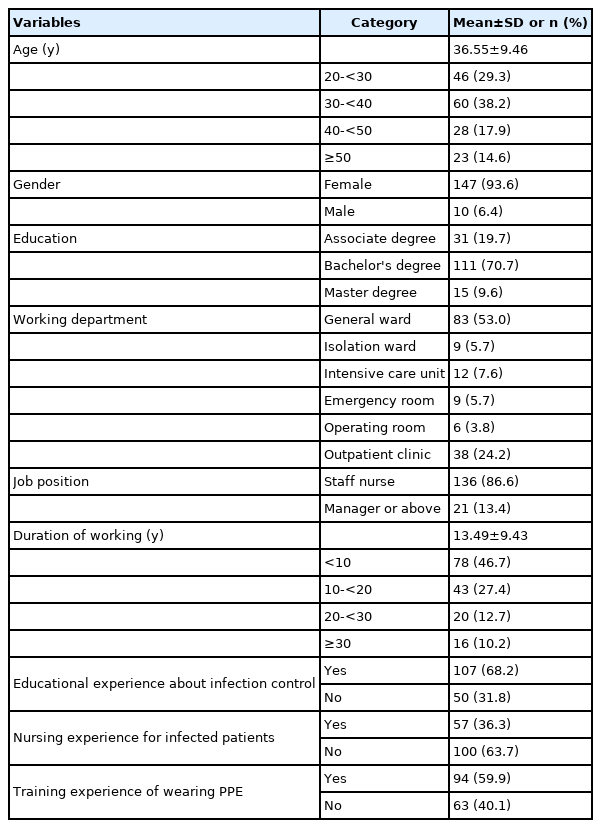
The average age of the subjects was 36.55 years old, and most nurses were in their 30s (38.2%). Regarding gender, females (93.6%) were more than males (6.4%). Most of the education levels were bachelor's degree (70.7%), and isolation ward, which department where the worked, accounted for only 5.7%. Staff nurses (86.6%) were much more than the manager above (13.4%), and the average duration of work was 13.49 years. 68.2% of nurses received infection control education before the outbreak of COVID-19, but only 36.3% had experienced nursing-infected patients, and 59.9% had experienced wearing PPE (Table 1).
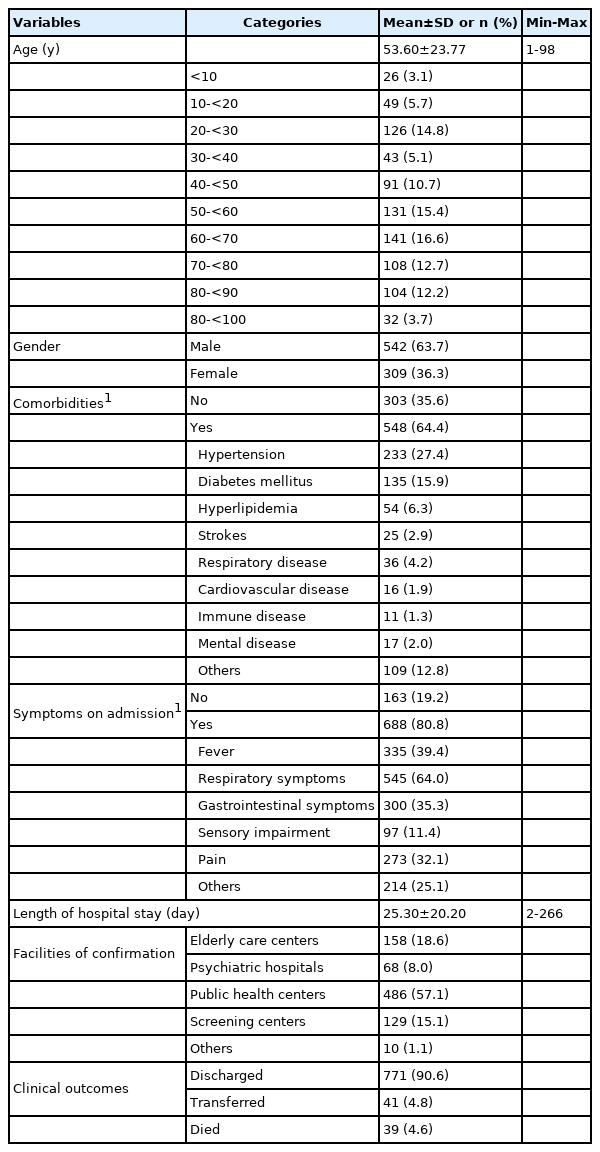
General characteristics of patients with COVID-19
The average age of 851 patients hospitalized with COVID-19 was 53.60 years, and the 60s were the most being, accounted 16.6%, but they were evenly distributed in various age groups from 1 to 98. In terms of gender, 63.7% were male, more than female, and 35.6% were without comorbidities. Hypertension (27.4%) and diabetes (15.9%) were the most common comorbidities due to multiple responses. At admission, 19.2% of subjects had no main symptoms. However, as a result of checking with multiple responses to the symptoms at admission, 545 (64.0%) had respiratory symptoms, 335 (39.4%) had to fever, 300 (35.3%) had gastrointestinal symptoms, and 273 (32.1%) had pain. The average length of hospital stay was 25.30 days and was distributed from a minimum of 2 days to a maximum of 266 days. Public health centers accounted for 57.1% of the facilities of confirmation, and the case of discharge after COVID-19 treatment was the most being, accounting for 90.6% (Table 2).
Nurses’ working status at a designated COVID-19 hospital
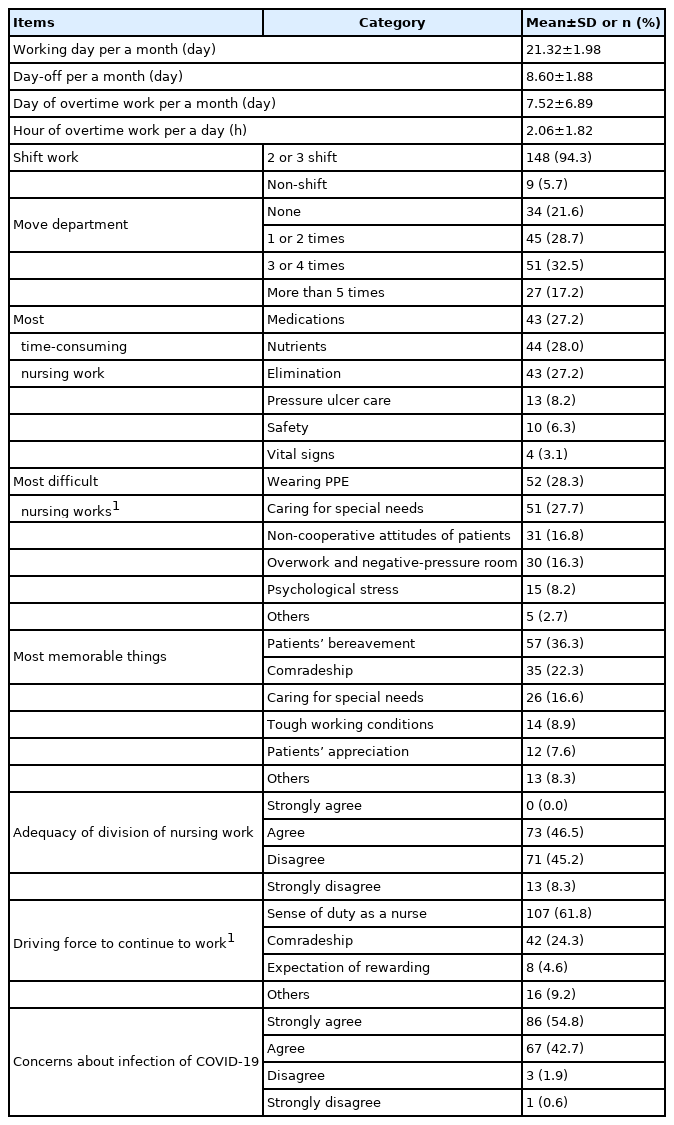
The average monthly working days were 21.32, and the day-off was 8.60 days per month. The average monthly overtime work was 7.52 days, and in the case of overtime, the 2.06 hours per month. Most of the types of work were 2 or 3 shifts with 94.3%, and transfer to another department during three months was the most common at 32.5% for 3 to 4 times. The nursing work that took the most time showed similar response rates for nutritional nursing related to providing meals (28.0%), medication (27.2%), and elimination (27.2%). The most difficult things in nursing patients with COVID-19 infectious diseases were wearing PPE (28.3%), caring for special needs (27.7%), the non-cooperative attitude of patients (16.8%), and so on. The most memorable moments were the bereavement of patients (36.3%) and comradeship (22.3%), and so on. Regarding the adequacy of work-sharing, 46.5% was ‘ appropriate’, which was very similar to 45.2% of ‘ not appropriate’. The driving force to continue to work as a nurse under challenging situations was the sense of duty as a nurse (61.8%) and comradeship (24.3%). Finally, for the concerns about infection of COVID-19, 54.8% of ‘ very worried’ and 42.7% of ‘ worried’ (Table 3).
Adequacy of support system for nurses working at a designated COVID-19 hospital
In response to the support system immediately after mass COVID-19 infection, 40.1% of respondents did not receive retraining on infection control and wearing PPE after the COVID-19 outbreak. Regarding the usefulness of the guidelines issued by the national and local governments that helped patient nursing care, ‘ disagree’ (51.0%) was higher than ‘ agree’ (49.0%). Most of the subjects disagree (77.1%) on whether the support from the government/local governments/institutions was sufficient. When asked about overtime, nurses responded that the amount of compensation (75.2%) and the timing of payment (89.2%) were not appropriate. In addition, regarding the adequacy of the amount of compensation (89.2%) and timeliness of payment of compensation (95.5%) for risky nursing work, respondents ‘ disagree’ (Table 4).
Nursing professional pride working at a designated COVID-19 hospital
The average nursing professional pride score was 3.44 points, and among the sub-factors, the score of ‘ Role of problem solver’ was the highest at 4.10 points. In addition, 91.7% of subjects responded that they felt that professional perception of nurses had improved compared to before the COVID-19 outbreak (Table 5).
DISCUSSION
The researchers investigated the experiences such as status of work, the adequacy of support system, and nursing professionals’ pride for nurses who worked at a designated COVID-19 hospital from February to May 2020 as the early pandemic as primary data for establishing an appropriate and systemic nurse working environment in the pandemic situation.
First, looking at the general characteristics of COVID-19 patients who directly affect nurses’ working environment. A total of 851 patients were hospitalized during the three months, and the average age was 53.60 years. The most common underlying diseases of COVID-19 patients were high blood pressure (27.4%) and diabetes (15.9%), and 90.6% were discharged from the hospital after hospitalization, but 4.8% were transferred to tertiary medical institutions, and 4.6% died. This result is similar to the results of a study by Hong et al. [19]; at the same time, 98 COVID-19 patients were admitted to tertiary medical; institutions. Among them, 5.1% died, and their average age was 55.4. In addition, most patients had respiratory symptoms (64.0%), other fever (39.4%), gastrointestinal symptoms (35.3%), and pain (32.1%), and 19.2% were asymptomatic, similar to the proportion of mild patients admitted to the residential treatment center [20].
In this study, the average working days of nurses dedicated to COVID-19 were 21.32 working days per month, 8.60 closed days, 7.52 overtime working days per month, and 2.06 overtime hours per day. Hospital where the study was conducted, could not accommodate all patients with COVID-19 infectious diseases rapidly increasing during the first pandemic, increasing the number of patients waiting for hospitalization. Therefore, existing general ward patients were sequentially discharged or transferred, and a panel door was installed from the first removed ward to create a ward. Then a mobile negative pressure device was installed in each ward and corridor to switch to a negative pressure ward. In addition, hospital facilities were reorganized so that isolated patients with advanced diseases could be cohort quarantined in negative pressure rooms and isolated patients with mild diseases from single negative pressure rooms to multi-person rooms. Finally, except for artificial kidney rooms, hospice centers, and minimal outpatient clinics, the entire ward was removed sequentially. Excluding the minimum number of nursing personnel, all nurses, including general wards, emergency rooms, intensive care units, neonatal rooms, delivery rooms, operating rooms, psychiatric wards, health examination centers, and screening teams, participated in direct nursing COVID-19 patients. Nevertheless, it was difficult to handle the rapidly increasing number of patient care only with the own nursing staff, so it was changed from three to two shifts from February 19 to February 28, 2020. Since then, due to the influx of dispatched personnel, it has been changed to three shifts from March 1. In addition, as temporary negative pressure wards were newly established one by one, changes in the workplace, shift hours, overtime, and overtime occurred. This is the same result as a study showing that 25% of Canadian nurses worked overtime during the COVID-19 pandemic in April and May 2020, and overtime hours were 9.7 hours per week in April and 10.3 hours per week in May [21]. In addition, this is the same result as 109 nurses working at 10 COVID-19 hospitals in China prefer to work four hours, but the actual working hours have been extended to five hours [22]. The subsequent most time-consuming nursing work for patients with COV-ID-19 infectious diseases was nutrition nursing helping patients eat and administrating medication, and the most challenging nursing work was wearing PPE. This is the same result as a study [22] in which 109 nurses working at a hospital dedicated to COVID-19 reported a lot of time wearing PPE, pain, dehydration, sweating, and other inconveniences caused by wearing PPE as a study [14] reported that people experience a lot of discomforts when wearing PPE and nursing patients directly. Above all, one of the findings to be noted in this study was that 97.5% of nurses were worried about infection with COVID-19 infection. This is the same result as a study [23–25] that reported that medical personnel who select and treat patients at the forefront when a new infectious disease occurs, especially nurses, have a very high risk of infection because they contact patients closer and longer. However, the main reason for continuing working without resigning was a sense of professional mission and fellowship even in such a complex working environment. This is similar to the result that was shown at the proud to be a nurse in the experiences of 43 nurses caring for COVID-19 patients [17]. In other words, the more complex the working environment was, the more nurses helped and relied on each other. As a result, they provide the best nursing care to patients by strengthening the cohesion and solidarity of the group. These results indicate the urgent need to prepare practical and actionable policies to properly utilize and deploy nursing personnel in a medical disaster such as a new infectious disease.
Meanwhile, 77.1% of nurses evaluated the appropriateness of the government/local government/institutional support system for nurses dedicated to COVID-19 as ‘ inappropriate’, and the amount and timing of support for overtime and risk allowances were ‘ inappropriate’. This is the same result as a study [14] that reported that no financial compensation or professional benefits were made for nurses in hospitals dedicated to COVID-19. In addition, about 40% of nurses answered that they were directly put into nursing without receiving retraining on infection control and wearing PPE after the outbreak of COVID-19. In a study by Lee et al. [26], which reviewed the strengths and weaknesses of nursing in the post-COVID environment through literature reviews, one of the weaknesses was the lack of face-to-face education and training, so it is necessary to provide regular and systematic infection control education for nurses in the future. In addition, Danesh et al. [27] 13 consider 22 studies related to difficulties in nursing work due to COVID-19 and suggest that appropriate support from institutions and society helps overcome the problematic situation of nursing patients with new infectious diseases. Hence, policies need to be established to improve this.
Finally, the nursing professional pride of nurses at COVID-19 dedicated hospitals revealed in this study was 3.44 points, and the score of the sub-factor of ‘ problem solver’ was the highest. This is similar to 3.52 points in a study [18] that developed a nursing professional pride tool for 294 nurses working in general wards and special departments. In particular, the sub-factor of ‘ problem solver,’ which had the highest score, is related to the professional work of nurses, which means that various patient needs are smoothly addressed. In other words, the higher the pride of nurses, the better they play the role assigned to them within the organization, and have a positive effect on improving the quality of nursing care services [18]. These results are the same as a study [28] that reported that 15 nurses in charge of rescue work for COVID-19 patients in tertiary hospitals experienced increased professional pride and a study [17] that reported that ‘ I felt proud of my job as a nurse’ in interviewing 43 nurses’ experiences.
Despite these results, the limitations of this study are as follows. First, this study was conducted in one designated COVID-19 hospital, so there is a limitation in generalizing the results of this study. Second, from February 18 to May 18, 2020, they participated in nursing patients with COVID-19 infectious diseases, but 26 nurses who left at the data collection were excluded from the study. However, since the number of people excluded from the study subjects is small, the study results’ impact is considered insufficient.
Based on the results of this study, it is suggested that it is necessary to prepare a policy to ensure a stable working environment for nurses no matter what unexpected new infectious diseases occur in the future.
CONCLUSION
This study attempted to investigate the experiences and the pride of nursing professionals of nurses working at a designated COVID-19 hospital during the early stage of the COVID-19 pandemic and use this as primary data to improve treatment and professional awareness. This study is a descriptive survey of 157 nurses who participated in nursing COVID-19 patients at the designated COVID-19 hospital when the number of COVID-19 patients exploded from February 18 to May 18, 2020. As a result of the study, nurses, who had to handle many patients with insufficient nursing personnel, worked an average of 21.32 days a month while working in two and three shifts and worked 7.72 days overtime a month, but 77.1% of nurses estimated that government and local government support was not appropriate. However, a sense of professional mission and fellowship was the driving force behind working without leaving the hospital in a challenging working environment. In addition, most nurses evaluated that they improved their perception of nurses through COVID-19. Furthermore, according to this study, nurses who take care of infectious disease patients at the forefront of the epidemic did extended work and worked overtime because wearing PPE and managing infectious diseases accompanied the more nursing tasks. Therefore, policies should be prepared to utilize nurse personnel and establish a government and local government support system.